
Written by Astrid Naranjo (Clean Health Accredited Clinical Dietitian)
Have you or your clients ever experienced bloating, wind and pain in the stomach?
You can thank FODMAPs!
FODMAP stands for:
Fermentable
Oligo
Di and
Monosaccharides
Polyols
They are small-chain of carbohydrates found in foods naturally or as food additives (1)
If your body is sensitive to FODMAPs, these can draw water into your intestine and rapidly ferment, so you’re guaranteed to feel bloated when you eat them!
IBS & FODMAPS what’s the relationship? Here are a few facts:
– Irritable bowel syndrome (IBS) affects around 1 in 7 people, with symptoms like(1):
- Lower abdominal pain
- Wind
- Bloating
- Changed bowel habit (ranging from diarrhea to constipation)
– 1 in 3 people with IBS are thought to have impaired digestion and absorption of one or more of ‘FODMAP’ foods (1,2)
– IBS symptoms can be reduced by 50% overall on the low FODMAP diet (3)
– Current evidence shows a diet low in FODMAPs is now used internationally, as the most effective dietary therapy for Irritable Bowel Syndrome (IBS) and symptoms of an irritable bowel (4,5)
– 1 million Australians consume gluten-free products. However, 90% of these people would feel just as good or better on a low FODMAP diet (4,5).
– A low FODMAP diet is, for the most part, designed to be done with guidance from a Dietitian (6-8)
– Fermentable carbohydrates are important for the healthy bacteria in your gut that benefits your health
– Only cut down FODMAPs as much as necessary and for as long as necessary to minimize symptoms (1,2)
There are 5 common ‘FODMAP’s found in food and what to look for on the label (2-5,15):
- FRUCTOSE: Found in fruit, honey, and fruit juices
- LACTOSE: Found in milk and milk products
- SUGAR POLYOLS: Xylitol, sorbitol, maltitol & mannitol: found in some fruits and vegetables, and are often used as artificial sweeteners
- FRUCTANS (FOS): Found in many grains like wheat and rye, and vegetables such as onions and garlic
- GALACTO-OLIGOSACCHARIDES (GOS) or GALACTANS: Found mainly in some vegetables and legumes.
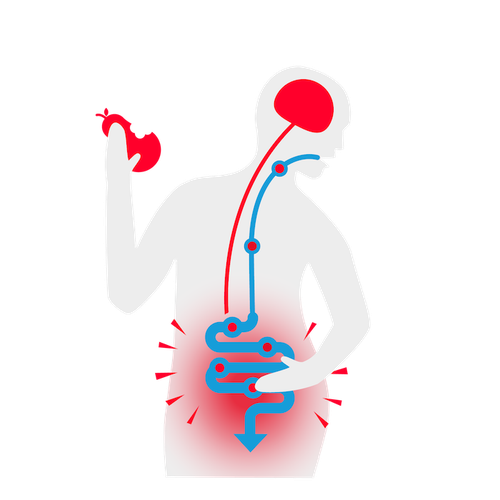
How are FODMAPs involved in triggering symptoms?
When we eat, food passes from the mouth down the oesophagus to the stomach. In the stomach, food is mixed and broken down before being slowly released into the small intestine. Enzymes in the small intestine continue to break food down to single molecules so that it can be absorbed across the wall of the small intestine into the blood stream (2-5).
Any part of food that isn’t broken down or absorbed in the small intestine will continue its path down the digestive tract and pass into the colon for elimination(1,2).
There are two processes that can occur during this process that influence IBS type symptoms:
FODMAP reactions occur in the colon, at the very end of the digestive tract. From the beginning to end (the mouth to the anus) the average adult digestive tract is about 9 meters long.
On average this means it takes about 6-24 hours from the time food is eaten until it reaches the colon where FODMAPs are fermented, resulting in IBS type symptoms (5-7).
1. Some FODMAPs are highly osmotic and draw water into the intestine. This can affect how fast the bowel moves, and cause diarrhea.
2. When FODMAPs reach the colon, they are fermented by the bacteria that naturally live there and just like when beer is fermented, this process creates gas and bubbles, resulting in abdominal distention,
bloating and cramping.
Gastro-colic reflex:
Why you may get symptoms within 30 minutes of eating, how can this happen?
This is known in medical terms as the “gastro-colic reflex”. At any point in time most people have about 24 hours or more worth of food in their digestive system. The reason symptoms can occur soon after eating is that when we chew, the gastro-colic reflex is triggered. This reflex tells the gut that more food is coming and it needs to move things along and make room. This then pushes food, that is sitting in the small bowel from an earlier meal, into the colon triggering symptoms fairly soon after a meal (2,3).
Can stress be a trigger?
Stress and anxiety can cause and exacerbate IBS symptoms. Stress hormones, put the nerve endings in your digestive tract into overdrive. This can increase in movement in the colon & can cause diarrhoea, even if FODMAPs aren’t present in the colon at the time. If you’re worried that eating an onion will cause you symptoms, it most probably will. It is quite easy to talk yourself into symptoms, so using mindfulness techniques or distraction to help manage this is a great strategy (2-5).
How long can symptoms last?
How long symptoms last is variable, from a few hours to a day or so. Many people also find that after a gut upset, it can take a few days to a week to feel normal again. There is no rush to go through challenges, doing them slowly and allowing any symptoms to settle before moving on will give more accurate results and be well worth it in the long run(1-4).
Who is a low FODMAP diet for?
Its primary use is to relieve digestion-related symptoms, but is emerging as a useful treatment tool for several other conditions too (5,7,10). It can be useful for those with:
- Irritable Bowel Syndrome (IBS)- more on that below
- Other forms of Functional Gastrointestinal Disorder (FGID)
- Small intestinal bacterial overgrowth (SIBO)
- Certain auto-immune conditions/diseases like (potentially) rheumatoid arthritis, multiple sclerosis or eczema
- Fibromyalgia or other health issues you’ve noticed are triggered by certain foods
- Frequent migraines that appear to be triggered after certain meals
There are 2 steps to follow a low FODMAP Diet This meal plan is highly restrictive and temporary (9,10).
- Low FODMAP diet: this diet needs to be strictly followed for 2-6 weeks or until symptom improvement has occurred.
- FODMAP Challenge process: after following the low FODMAP diet the FODMAP groups will be introduced back into the diet over a period of 6-8 weeks.
The most common outcome of this 2-stage process is that your IBS-type symptoms will be minimized, while tolerating increased variety of foods in an eating plan that is individualized.
6 Important Key Tips to know before you jump on a Low FODMAP diet:
- It is NOT appropriate for certain medical conditions: That includes people with diet-related medical conditions (eg. type 1 or type 2 diabetes using medication) and those at risk of eating disorders or emotionally fragile. Also it goes without saying that this is not for children- any elimination diet for a child must be under direct supervision of a dietitian.
- Choose water as your drink: keep a bottle of water with you at all times and drink up. Black coffee, black tea, peppermint tea, and green tea are very low FODMAP and okay to have (milk isn’t recommended).
- Portion size is fundamental: Most low FODMAP foods still contain small amounts. For example, a serving of pineapple is low FODMAP, but if you eat half a pineapple in one go then your FODMAP intake will be high.
- Prepare all foods yourself at home where possible: To avoid accidentally consuming high FODMAP foods usually means planning meals ahead of time.
- Keep a food diary: Record each meal you had and if you experienced any undesirable symptoms after each meal or later that day. This is known as a food diary and is crucial for helping you recognise triggers and later on for the reintroduction phase.
- Download and purchase the Monash University FODMAPs app (11), available on iPhone and Android devices. They have a huge bank of foods that have been tested for their FODMAP levels, as well as almost 100 original recipe ideas.
Strategic Low FODMAP dining out options
Set meal plans aren’t particularly useful when you’re eating out at a restaurant or takeaway shop. Here are some food choice tips to help you make appropriate choices (11-14):
- Ask for gluten-free bread (preferably white)
- Lactose-free yogurt served with low FODMAP fruits (Greek yogurt is okay too but still has some FODMAPs)
- Coffee or tea with lactose-free milk
- Breads or cereals made from oats for breakfast
- Smoothies made with lactose-free milk and low FODMAP fruits and vegetables
- Low FODMAP salad with nuts, seeds, extra virgin olive oil & fresh squeezed lemon
- Roasted, steamed or grilled low FODMAP vegetables
- Choose meat, fish, egg or tofu dishes that are plain (separate from sauces/gravies)
- Chicken with egg mayonnaise or beef with mustard
- Small French fries is okay at fast-food restaurant (although not encouraged obviously)
- Carrot and cucumber sticks with hummus as starter or snack
- Curry dishes with rice is generally okay, but it depends on the curry paste used.
- Popcorn at the cinema
- Sushi and sashimi with soy sauce and wasabi
- When traveling, fill a thermos with lactose-free milk or almond milk to add to oats/oatmeal.
Take Home Points
- FODMAPs are sugars commonly found in everyday foods.
- Dietary restriction of FODMAPs may improve IBS symptom control.
- Speak with your health care professional to ensure other gastrointestinal conditions have been investigated prior to changing your diet.
- Work with a dietitian to develop a personal eating, shopping and dining-out plan.
- This diet is usually recommended for 2-6 weeks. Once symptoms settle foods may be gradually re-introduced.
- A strict low FODMAP diet should NOT be followed long term.
To learn how to blend the science & practical application of nutrition to create safe, effective and results based diets for clients, click here & enrol into the Performance Nutrition Coach Certification Collection!
References
- Gibson et al (2015). Food components and Irritable Bowel Syndrome. Gastroenterology. 148:1158-74 e4.
- Shepherd SJ, Parker FJ, Muir JG and Gibson, PR Dietary triggers of abdominal symptoms in patients with irritable bowel syndrome- randomised placebo-controlled evidence Clin. Gastroenterol. Hepatol. 2008;6(7):765-771. http://www.sciencedirect.com/science/article/pii/S1542356508001511
- Halmos, EP, Power VA, Shepherd SJ, et al. A Diet Low in FODMAPs Reduces Symptoms of Irritable Bowel Syndrome. Gastroenterology 2014;146(1)67-75
- Canavan et al (2014). The epidemiology of irritable bowel syndrome. Clin Epidemiol 6:71-80.
- Marsh et al (2016). Does a diet low in FODMAPs reduce symptoms associated with functional gastrointestinal disorders? A comprehensive systematic review and meta-analysis. Eur J Nutr 55:897-906.
- The Low FODMAP Diet: Healthy Eating Guidelines. 2016 Dietitians of Canada
- McKenzie et al (2016). British Dietetic Association systematic review and evidence-based practice guidelines for the dietary management of irritable bowel syndrome in adults (2016 update).J Hum Nutr Diet 29:549-75.
- Monash University, Low FODMAP Diet Dietitians Workshop (2016)
- National Institute of Health and Care Excellence (2008). Irritable bowel syndrome in adults:diagnosis and management. NICE guideline (CG61).
- Shepherd, S. Gibson, P. (2006) Fructose Malabsorption and symptoms of Irritable Bowel Syndrome: Guidelines for EFGective Dietary Management. J Am Diet Assoc 2006; 106:1631-1639.
- FODMAP Friendly smartphone app: http://fodmapfriendly.com/app/
- FODMAPs. http://www.fodmapped.com/fodmaps/
- Martin, L (2016). Re-challenging and Reintroducing FODMAPs A self-help guide to the entire reintroduction phase of the low FODMAP diet.
- Tuck, C. Barrett, J. (2017). Re-challenging FODMAPs: the low FODMAP diet phase two, J Gastroenterol Hepatol. 2017 Mar;32 Suppl 1:11-15. doi: 10.1111/jgh.13687.
- Jaci Barrett, APD et al.(2013). Low FODMAP Diet To improve Irritable Bowel Syndrome (IBS) symptom control. Digestive Health Foundation SECOND EDITION 2013. Available https://www.gesa.org.au/public/13/files/Consumer%20Information/Low%20FODMAP%20Diet%202nd%20Ed.pdf






